
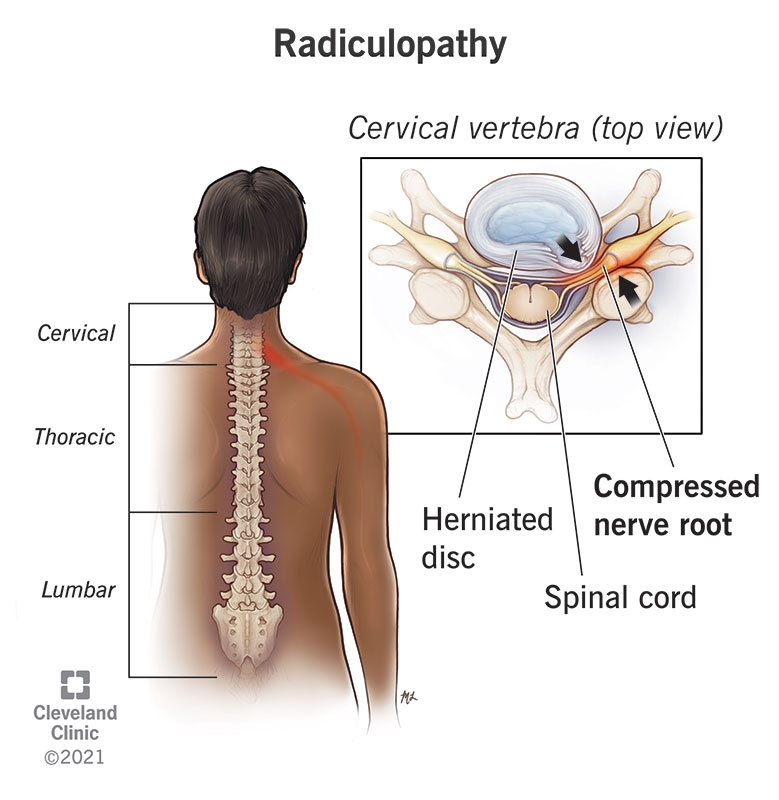
Nerve root compression causing radiating symptoms.
When you have cervical disc herniation, one of the cushioning discs between the bones in your neck has developed a problem. Think of these discs like jelly donuts - they have a tough outer ring and a soft, gel-like center called the nucleus pulposus. When a disc herniates, this soft inner material pushes out through a weak spot in the outer ring, similar to jelly squeezing out of a donut.
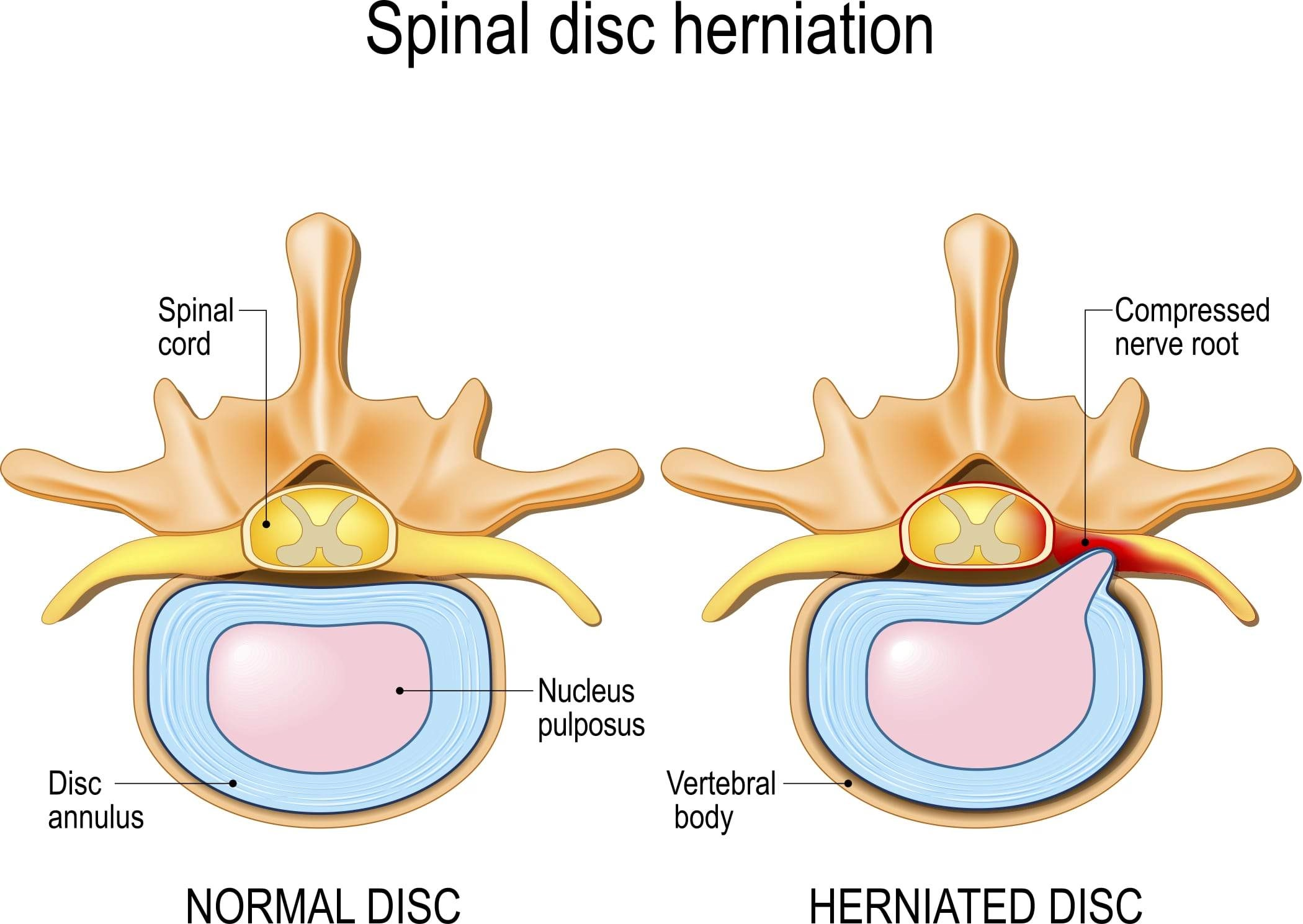
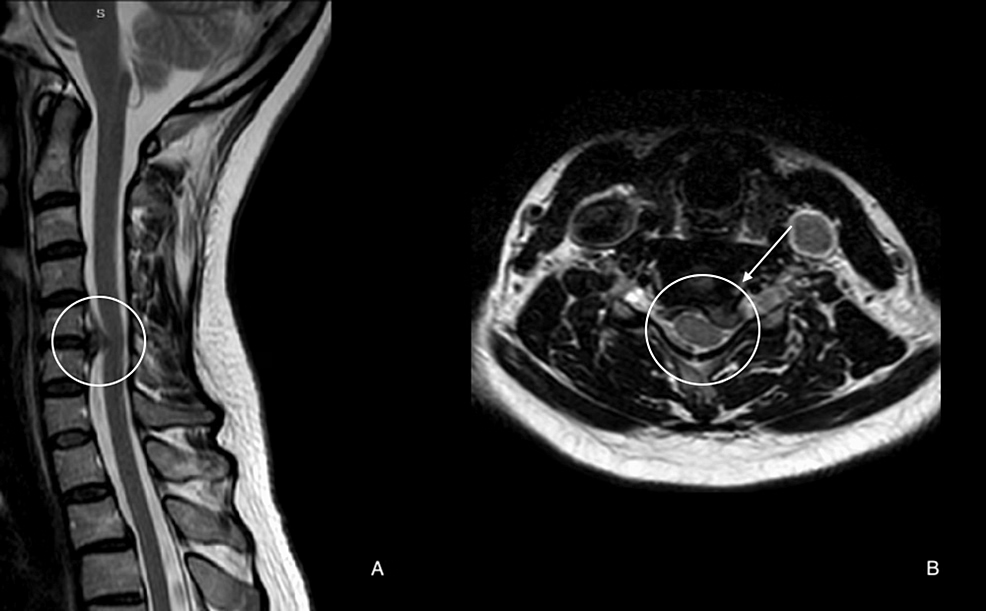
This herniated disc material can then press against or irritate the nerve roots that branch off from your spinal cord in your neck. When this happens, doctors call it cervical radiculopathy - essentially meaning that a nerve root in your neck area is being compressed or irritated. Among the different ways nerves can become compressed in the neck, sideways (lateral) disc herniations rank as the second most common cause.
Doctors primarily diagnose cervical radiculopathy by carefully listening to your symptoms and examining you. The most common signs include:
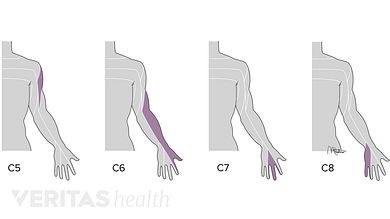
Pain That Travels a Specific PathYou'll likely experience neck pain that radiates down into your arm and fingers. This pain follows specific pathways called dermatomes, which help your doctor identify which nerve is being affected.
Unusual Sensations in Your Arm and HandMany patients describe tingling, numbness, or "pins and needles" sensations in their arm and hand. These aren't just minor inconveniences - they're important clues about which nerve is being compressed.
Changes in How Things FeelYou may notice that your sense of touch becomes altered in certain areas of your arm or hand. Some spots might feel numb, while others might be overly sensitive.
Weakness in Specific Muscle GroupsThe herniated disc can interfere with nerve signals that control certain muscles, leading to weakness that follows predictable patterns.
Reduced ReflexesDuring examination, your doctor will test reflexes. When a nerve root is compressed, the reflexes it controls often become diminished or absent.
Most patients notice that certain activities make their arm pain or tingling worse. Any movement or action that increases pressure within your spinal canal - such as coughing, sneezing, or certain neck movements - often intensifies the symptoms.
Interestingly, many patients find that their arm pain is actually more bothersome than their neck pain. Some people have significant arm symptoms with only mild neck discomfort.
The C7 nerve root is by far the most frequently compressed, accounting for approximately 46-69% of all cases. The C6 nerve root is the second most commonly affected, representing about 17-20% of cases. C5 and C8 nerve roots are less frequently involved in disc herniation.
While age-related wear and tear of the spine typically affects older individuals, cervical disc herniation actually occurs more frequently in younger patients. The development usually results from multiple factors working together over time.
Gender: Men are more likely to develop cervical disc herniation than women.
Smoking: Current cigarette smoking is one of the most important modifiable risk factors. Smoking damages the blood vessels that supply nutrients to your discs, making them more susceptible to breakdown. Smokers are nearly three times more likely to develop cervical disc herniation.
Occupational Hazards: Certain professions carry elevated risk, including military aviators, professional drivers, and workers who operate vibrating equipment.
Physical Activities: Heavy lifting and frequent diving from a board have been identified as risk factors.
Trauma: While commonly assumed to be a major cause, only about 15% of patients report a history of trauma preceding their symptoms. This means 85% of cases develop without any identifiable traumatic trigger.
Current research hasn't definitively established factors like poor posture, repetitive neck movements, or genetic predisposition as direct causes of cervical disc herniation, though they may affect general neck health.
Your cervical spine contains intervertebral discs that act as shock absorbers. The openings where nerve roots exit (intervertebral foramina) are funnel-shaped, with the entrance being the narrowest part. This creates a bottleneck effect - even small disc herniations can cause significant nerve compression.
The middle and lower cervical regions are particularly susceptible to problems because they experience the greatest combination of mobility and stress. This is why disc herniations commonly occur at levels like C5-C6 and C6-C7.


Your cervical spine's narrow spaces make nerve roots particularly vulnerable to compression. Modern MRI technology allows doctors to measure exactly how much a disc protrusion reduces available space. When disc protrusions compromise more than one-third of the spinal canal's diameter, this typically correlates with symptoms.
Not everyone has the same canal dimensions. Some people naturally have more spacious canals, while others have smaller spaces. This variation helps explain why people with similar disc problems might have different symptom severity.
Physiotherapy is widely recognized as a cornerstone of conservative management for cervical disc herniation. Research consistently shows favorable outcomes for most patients who pursue conservative treatment approaches.
The outcomes research is quite encouraging:
The natural course of cervical disc herniation is generally favorable, and disc herniations often resolve spontaneously. Most patients experience substantial improvements within the first 4-6 months, with complete recovery occurring in approximately 83% of patients within 24-36 months.
Surgery is typically reserved for patients with persistent pain after 6-12 weeks of conservative therapy or when there's evidence of progressive motor weakness. Importantly, research shows no significant long-term differences between conservative and surgical approaches in comparative studies.
Most patients initially present with intense pain and moderate disability. The initial pain and inflammation typically peak in the first 1-2 weeks, but significant improvement in pain levels often occurs within 4-6 weeks. Research shows 75% of patients experience pain relief at 4 weeks across various treatment approaches.
Substantial improvements in pain and disability tend to occur within the first 4-6 months post-onset. During this period, most patients notice their daily function improves significantly.
Complete recovery occurs in approximately 83% of patients within 24-36 months. Muscle strength typically returns to normal by 36 months. None of the patients in research studies developed progressive neurologic deficits or worsening problems long-term.
Treatment Adherence: Patients who follow prescribed treatment programs have significantly better outcomes, with 92% returning to full work duties.
Smoking: Adversely affects disc nutrition and healing capacity.
Occupational Factors: Patients with workers' compensation claims may have slower recovery.
Recover faster, move better, and feel stronger with expert physiotherapy. Our team is here to guide you every step of the way.

Goals: Pain reduction and inflammation control while supporting natural healing.
Assessment includes:
Treatment focuses on:
Goals: Restore mobility, begin strengthening, improve posture.
Treatment includes:
Important note: Research shows insufficient evidence for manipulative techniques in cervical radiculopathy, and cervical manipulation carries risks of serious complications.
Based on research evidence, effective prevention focuses on:

Exercise therapy is one of the most widely used interventions for cervical problems. Prevention programs should include:
Smoking Cessation: The most important modifiable risk factor. Smoking adversely affects vertebral blood supply, leading to decreased disc nutrition. This is the single most impactful prevention intervention.
Note: While factors like stress management, weight management, and adequate sleep are beneficial for overall health, current research hasn't specifically established them as direct prevention strategies for cervical disc herniation.
Understanding these evidence-based facts about cervical disc herniation empowers you to make informed decisions about your care and maintain realistic expectations throughout your recovery journey.
If you're experiencing neck pain that travels down your arm, you may be dealing with cervical radiculopathy—a condition that sounds complicated but is actually quite common and treatable. Think of your spine as a highway system where nerves travel from your brain to different parts of your body. Cervical radiculopathy occurs when one of these nerve "highways" gets squeezed or compressed in your neck area.
This compression typically happens for two main reasons:
When these nerves get compressed, you might experience:
The pattern of these symptoms follows specific "nerve maps" called dermatomes (for sensation) and myotomes (for muscle function). You might notice that certain movements—like turning your head, coughing, or sneezing—make the pain worse because they increase pressure around the compressed nerve.
Your healthcare provider will primarily rely on a thorough clinical examination and your symptom description to diagnose cervical radiculopathy. This hands-on approach is often more telling than any single test.
Physical Examination Techniques:Your doctor may perform several specific tests during your visit:
Advanced Imaging and Testing:While the clinical examination is paramount, your doctor may recommend additional tests to confirm the diagnosis and rule out other conditions:
Here's the most important information you need to know: cervical radiculopathy due to disc herniation has an excellent natural recovery rate. Medical research consistently shows that the human body has remarkable healing capabilities when it comes to this condition.
Timeline for Improvement:
What About Recurrences?Research shows that about 22% of patients may experience some recurrence of moderate pain over a 24-36 month period. However, these recurrent episodes are typically:
Reassuring Long-term Outlook:Studies following patients over extended periods have found no cases of progressive neurological deterioration or development of myelopathy (spinal cord compression). This means that while you may experience symptoms now, your condition is very unlikely to progress to more serious neurological problems.
This favorable natural history means that most treatment approaches focus on managing symptoms during the healing process rather than attempting to "fix" the underlying disc herniation, which often resolves on its own through the body's natural healing mechanisms.
The excellent news about cervical radiculopathy is that non-surgical treatment is highly effective and represents the recommended first-line approach for most patients. Since your body has such strong natural healing capabilities for this condition, conservative care focuses on supporting your recovery while managing symptoms during the healing process.
Why Exercise Therapy Works:Exercise therapy stands out as one of the most widely utilized and effective interventions for cervical radiculopathy. Rather than simply resting and waiting for improvement, targeted exercises can accelerate your recovery and prevent future episodes.
Components of Your Rehabilitation Program:
Comprehensive Strengthening Protocol:
Progressive Neck Mobilization:Your therapist will gradually introduce controlled neck movements that help restore normal range of motion while respecting your healing tissues. This progressive approach prevents stiffness while avoiding aggravation of your symptoms.
Education and Postural Rehabilitation:Perhaps most importantly, you'll learn about proper cervical spine mechanics—how your neck should move and be positioned during daily activities. This education component often prevents future recurrences and empowers you to take control of your recovery.
Ergonomic Awareness and Daily Living Adaptations:Your recovery extends far beyond formal exercise sessions. Learning proper body mechanics involves understanding how to position your neck during everyday activities—whether you're working at a computer, reading, driving, or sleeping. Key principles include avoiding prolonged static postures, using proper lifting techniques that protect your neck, and being mindful of your head and neck position throughout the day.
Smoking Cessation: A Critical Recovery Factor:If you smoke, quitting represents one of the most important steps you can take for your cervical spine health. Smoking is a significant risk factor for disc problems because it impairs blood supply to your vertebrae and reduces nutrition to your spinal discs. This interference with natural healing processes can significantly slow your recovery and increase the likelihood of future problems.
Pain Relief Medications:Most patients will be prescribed analgesics (pain relievers) to help manage discomfort during the acute phase of their condition.
Anti-Inflammatory Medications: What the Research Shows:While inflammation is suspected to play a role in radiculopathy, it's important to understand that current medical research shows no strong evidence supporting the effectiveness of non-steroidal anti-inflammatory drugs (NSAIDs) or oral corticosteroids for cervical radiculopathy. This doesn't mean these medications are harmful, but rather that their benefits may be limited compared to other treatment approaches.
When Collars May Help:Cervical collars are often prescribed during the acute or subacute stages of your condition (typically the first few weeks). The theory is that limiting neck movement can reduce pain by minimizing nerve root irritation.
Important Limitations and Risks:However, the effectiveness of cervical collars is actively debated in medical literature. Some studies show no benefit for persistent radiculopathy symptoms. More concerning is that prolonged collar use can lead to adverse effects, particularly weakening (atrophy) of the important muscles that support your neck. For this reason, if a collar is prescribed, it's typically recommended for short-term use only.
The Current Evidence:Periradicular or epidural corticosteroid injections represent a more invasive treatment option. While some earlier observational studies suggested favorable results, helping patients avoid surgery, recent high-quality randomized controlled studies have failed to demonstrate positive effects.
Understanding the Risks:These procedures carry both minor risks (temporary increase in pain at the injection site) and rare but serious complications including anterior spinal artery syndrome and cerebellar strokes—both potentially life-altering conditions. Given the lack of strong evidence for benefit combined with these potential risks, most spine specialists do not routinely advocate for these injections without compelling research support.
Limited Evidence for Benefit:Current medical literature shows insufficient evidence to support the effectiveness of manipulative techniques specifically for cervical radiculopathy patients.
Significant Safety Considerations:Cervical spine manipulation carries documented risks of serious complications, including vertebral artery dissection and spinal cord compression. These risks are particularly concerning when appropriate imaging (like MRI) hasn't been performed to fully understand your specific anatomy and condition. For these safety reasons, manipulation is generally discouraged as a treatment approach for cervical radiculopathy.
The Bottom Line on Conservative Treatment:The most effective conservative approach combines evidence-based physical therapy, lifestyle modifications, and appropriate pain management while avoiding potentially risky interventions that lack strong scientific support. This comprehensive approach aligns perfectly with your body's natural healing timeline and maximizes your chances of complete recovery.
While the vast majority of patients with cervical radiculopathy recover with conservative treatment, it's crucial to recognize when professional medical evaluation or more intensive treatment might be necessary. Understanding these warning signs empowers you to make informed decisions about your care.
Intractable or Persistent Pain:If you're experiencing severe pain that doesn't respond to initial conservative treatment approaches, medical evaluation is warranted. Pain that remains unchanged despite appropriate rest, activity modification, and basic pain management strategies may require professional assessment to ensure you're receiving optimal care.
Extended Pain Duration:Medical research suggests that if your pain persists after 6 to 12 weeks of conservative therapy, it's time to consult with a healthcare provider. This timeframe is significant because most cases of cervical radiculopathy show substantial improvement within this period. Persistent symptoms may indicate the need for more specialized treatment approaches or additional diagnostic evaluation.
Progressive Neurological Symptoms:Perhaps most importantly, you should seek immediate medical attention if you notice:
Signs of Spinal Cord Compression (Myelopathy):This represents a medical emergency requiring immediate evaluation. Warning signs include:
Here's reassuring perspective: surgery is rarely needed for cervical disc herniation. Medical literature shows that only approximately 26% of patients with cervical radiculopathy ever require surgical intervention. This statistic underscores that conservative care is not only the first-line treatment—it's also successful for the vast majority of patients.
When Surgery Might Be Considered:Surgical intervention is typically reserved for cases involving:
Conservative Care Remains the Foundation:Even in cases where surgery is eventually considered, conservative treatment almost always represents the initial approach. This gives your body the best opportunity to heal naturally while providing valuable information about how your condition responds to non-invasive interventions.
Progressive Neck Mobilization: The Supported ApproachResearch specifically supports progressive neck mobilization as an effective component of comprehensive cervical radiculopathy treatment. This technique involves gentle, controlled movements that gradually restore normal range of motion while respecting your body's healing timeline.
Key Benefits of Mobilization:
The Critical Distinction: Mobilization vs. ManipulationIt's essential to understand the important difference between mobilization and manipulation:
Mobilization involves gentle, controlled movements within your comfortable range of motion. These techniques are supported by research and carry minimal risk when performed by trained professionals.
Manipulation, however, involves high-velocity, low-amplitude thrusts that can carry significant risks. Current research shows insufficient evidence for effectiveness of manipulative techniques in cervical radiculopathy patients. More concerning, cervical spine manipulation carries documented risks of serious complications including:
These risks are particularly elevated when appropriate imaging hasn't been performed to understand your specific anatomical situation. For these safety reasons, manipulation is generally discouraged for cervical radiculopathy treatment.
While the term "neurodynamic treatment" encompasses various specialized techniques not explicitly detailed in current research literature, the underlying principle—reducing nerve root irritation and improving neurological function—aligns perfectly with evidence-based treatment goals for cervical radiculopathy.
Understanding Neurodynamic Principles:These treatment approaches focus on:
Integration with Comprehensive Care:When neurodynamic techniques are employed, they work most effectively as part of a comprehensive treatment program that includes postural education, strengthening exercises, and activity modification rather than as standalone interventions.
The Importance of Evidence-Based Practice:While specialized manual therapy techniques may offer benefits, it's crucial that any treatment approach you receive is grounded in current research evidence and delivered by practitioners who understand both the potential benefits and limitations of these interventions.
Making Informed Treatment Decisions:The most effective approach to cervical radiculopathy treatment combines techniques with strong research support while avoiding interventions that carry significant risks without proven benefits. This evidence-based approach maximizes your chances of complete recovery while minimizing the risk of complications or prolonged symptoms.
The Foundation of Long-term Success:Research consistently demonstrates that education on proper cervical spine mechanics and postural rehabilitation represent integral components of effective physical rehabilitation programs for cervical radiculopathy. These aren't just add-on services—they're fundamental elements that can prevent future recurrences and accelerate your current recovery.
Comprehensive Postural Assessment:Effective postural correction begins with understanding how your current posture contributes to nerve compression and pain. This involves analyzing your sitting, standing, and sleeping positions, as well as how you perform daily activities. Common postural issues that contribute to cervical radiculopathy include:
Workplace Ergonomic Assessments: Your Daily Environment MattersSince many people spend 8+ hours daily at workstations, workplace ergonomics play a crucial role in both recovery and prevention. Research emphasizes instruction in body mechanics and adaptation of daily living principles as essential for managing cervical radiculopathy.
Key Ergonomic Factors Include:
Beyond the Workplace:Ergonomic principles extend to all daily activities—driving positions, reading habits, smartphone use, and recreational activities. Understanding how to modify these activities protects your healing tissues while preventing future problems.
Evidence-Based Strength Training:Research strongly supports supervised active general upper and lower extremity strengthening and endurance combined with thoracic spine stabilization training as core components of cervical radiculopathy rehabilitation. However, the key word here is "supervised"—these aren't generic exercises but carefully progressed programs tailored to your specific needs and recovery stage.
Multi-Level Strengthening Approach:
Phase 1: Foundation Building
Phase 2: Functional Integration
Phase 3: Advanced Functional Training
Thoracic Spine Stabilization: The Hidden KeyMany patients don't realize that thoracic (upper back) strength directly impacts cervical spine health. A strong, stable thoracic spine provides the foundation that allows your cervical spine to function optimally. This connection explains why comprehensive programs address the entire kinetic chain rather than focusing solely on the neck.
Dry Needling for Muscle Tension and Trigger Points:While dry needling isn't specifically mentioned in current cervical radiculopathy research literature, this technique addresses muscle tension and trigger points that often accompany nerve compression conditions. When considering any treatment not explicitly studied for cervical radiculopathy, it's important to evaluate:
Individual Treatment Customization:The principle of tailoring treatments to individual needs represents a fundamental aspect of effective rehabilitation. Your specific symptoms, functional limitations, work demands, recreational goals, and healing timeline all influence the optimal treatment approach. This individualized strategy aligns perfectly with research showing that comprehensive, personalized conservative care achieves positive outcomes in approximately 83% of patients.
Aligning with Natural Recovery:Remember that cervical radiculopathy has a generally favorable natural course, with substantial improvements typically occurring within 4-6 months and complete recovery achieved in approximately 83% of patients over 24-36 months. The most effective treatment approaches work with this natural healing timeline rather than against it.
The Comprehensive Advantage:Programs that combine evidence-based exercise therapy, postural correction, ergonomic training, and individualized rehabilitation represent the gold standard of conservative management. This multifaceted approach addresses not just your current symptoms but also the underlying factors that contributed to your condition, maximizing both your immediate recovery and long-term spine health.
Evidence-Based Decision Making:As you consider treatment options, prioritize approaches with strong research support while being cautious of interventions that carry significant risks without proven benefits. The goal is to achieve complete recovery through the safest, most effective means possible.
Book Your Comprehensive Assessment Today
Phone: 905-669-1221
Location: 398 Steeles Ave W #201, Thornhill, ON L4J 6X3
Online Booking: www.vaughanphysiotherapy.com
Don't let neck pain control your life. Our experienced physiotherapists specialize in evidence-based cervical radiculopathy treatment and will work with you to develop a personalized recovery plan that addresses your specific needs, work demands, and lifestyle goals. From comprehensive postural assessments to progressive strengthening programs, we're committed to helping you achieve complete recovery and preventing future recurrences.
Ready to start your journey back to pain-free living? Contact us today to schedule your detailed assessment and begin your evidence-based recovery program.
Written by Sophie Lee
Explore the latest articles written by our clinicians