
Inner ear infection causing vertigo and balance disturbances.
Think of your inner ear as a sophisticated navigation system housed in a small, spiral-shaped structure called the labyrinth. When you have labyrinthitis, this entire system becomes inflamed and swollen, affecting both your ability to hear and maintain balance.
The labyrinth contains two essential components working together: the cochlea (responsible for hearing) and the vestibular system (responsible for balance). When inflammation strikes both areas simultaneously, patients typically experience the "double trouble" of spinning sensations (vertigo) combined with hearing difficulties. This dual impact is what distinguishes labyrinthitis from other inner ear conditions.
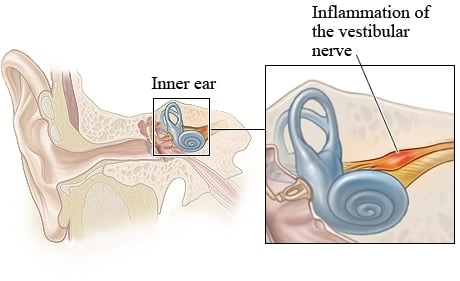
Vestibular neuritis (sometimes called vestibular neuronitis by medical professionals) involves inflammation of a specific nerve pathway—the vestibular nerve. Picture this nerve as a crucial communication cable that constantly sends balance information from your inner ear's motion sensors to your brain's balance control center.
When this nerve becomes inflamed, the communication between your inner ear and brain becomes disrupted or "scrambled," leading to intense dizziness and balance problems. However, because the hearing portion of your inner ear remains unaffected, vestibular neuritis characteristically causes severe vertigo without any hearing loss. This preservation of hearing while experiencing significant balance disruption is a key identifying feature that helps healthcare providers distinguish it from labyrinthitis.
From a medical perspective, vestibular neuritis represents what specialists call an "acute peripheral vestibulopathy"—essentially a sudden-onset condition affecting the balance organs outside the brain. It ranks as the third most frequently encountered peripheral vestibular disorder, occurring less commonly than benign paroxysmal positional vertigo (BPPV) and Ménière's disease, but still affecting a significant number of patients annually.
Advanced medical research using specialized tissue analysis (histopathological studies) has revealed the precise anatomical changes in vestibular neuritis. The inflammation specifically targets three interconnected structures:
Medical experts classify this as a "mononeuropathy"—meaning it affects a single nerve pathway. Importantly, the inflammation occurs in the nerve itself, positioned between the inner ear structures and the brain, rather than directly damaging the delicate inner ear organs. This explains why hearing typically remains intact while balance function becomes severely compromised.
This targeted nerve inflammation creates a temporary "communication breakdown" between your perfectly functioning inner ear balance organs and your brain's balance processing centers, resulting in the characteristic symptoms patients experience.
While these conditions can be incredibly disruptive to your daily life, the medical community is still working to fully understand their exact origins. What we do know is that the precise cause remains somewhat of a medical puzzle, but decades of research have identified several important pieces that help explain why some people develop these conditions.
The Viral ConnectionThe most widely accepted explanation points to viral infections as the primary culprit. Think of it this way: just as a computer virus can disrupt your device's normal operations, certain viruses can interfere with your inner ear's delicate functioning.
Common Cold and Flu LinksBoth labyrinthitis and vestibular neuritis frequently develop following what seems like an ordinary cold or flu. This isn't coincidental—these common viral infections can sometimes "travel" to affect your inner ear structures. Research shows that between 43% and 46% of people with vestibular neuritis had a recent upper respiratory tract infection, suggesting a clear connection between these everyday illnesses and inner ear problems.
The Herpes Simplex Connection: A Hidden ResidentHere's where the science gets particularly fascinating: Herpes simplex virus type 1 (HSV-1) appears to be the most common viral cause of vestibular neuritis. Before you worry, this is the same virus that causes cold sores and is present in most adults without causing problems.
Medical research has discovered HSV-1 genetic material in about two-thirds of human vestibular nerve clusters examined during medical studies. Scientists believe this virus can remain "dormant" or inactive in your nerve tissue for years, like a sleeping dragon. When your immune system becomes stressed or weakened (perhaps by another illness), this dormant virus can "reactivate," causing inflammation and swelling that damages the vestibular nerve cells and their connecting fibers.
Why Some Nerves Are More VulnerableInterestingly, medical imaging studies have revealed that the superior vestibular nerve is more prone to problems than its counterpart, the inferior vestibular nerve. This vulnerability stems from anatomy: the superior nerve must travel through a narrower and longer bony tunnel in your skull. When inflammation occurs, this tight space creates a "traffic jam" effect, making the nerve more susceptible to damage from swelling or reduced blood flow.
Vascular ComplicationsAnother compelling theory involves problems with blood circulation to your inner ear. Your vestibular system, like all body parts, depends on a steady blood supply through tiny vessels. Some researchers propose that reduced blood flow to the anterior vestibular artery (a small but crucial blood vessel) might trigger vestibular neuritis.
The Inflammatory CascadeAdvanced laboratory studies have discovered that patients with vestibular neuritis show signs of widespread inflammation in their blood cells. Specifically, certain immune cells called monocytes and macrophages become overactive. This creates what scientists call a "pro-inflammatory state"—imagine your body's defense system being stuck in overdrive.
This excessive inflammation may cause microscopic blood clots or reduce blood flow to the delicate vestibular organs, essentially "starving" them of oxygen and nutrients. However, when researchers examine tissue samples, they don't always find clear evidence of blocked blood vessels, suggesting this mechanism might be more complex than originally thought.
When Your Body Attacks ItselfPerhaps the most intriguing recent development in understanding these conditions involves immune-mediated mechanisms—essentially, your immune system mistakenly attacking your own inner ear structures.
The Timing ClueMedical observation provides an important clue: there's often a gap between when people get sick with a respiratory infection and when their vestibular symptoms begin. This timing pattern suggests that rather than the virus directly attacking the inner ear, the problem might be your immune system's delayed response to the infection going awry.
The Multiple Sclerosis ConnectionResearch has revealed striking similarities between vestibular neuritis and multiple sclerosis, another condition where the immune system attacks nerve tissue. In both conditions, patients show an imbalanced ratio of different types of immune cells—specifically, too few "suppressor" cells that normally prevent immune overreactions.
This imbalance may allow what scientists call "forbidden clones" of immune cells to become active. These rogue cells potentially produce antibodies that mistakenly target your own vestibular nerve tissue, treating it as if it were a foreign invader. This would classify vestibular neuritis as an autoimmune condition, similar to other diseases where the body attacks itself.
While viral infections dominate the research, other factors can occasionally trigger these conditions:
Bacterial Infections: Less commonly, bacterial infections can cause labyrinthitis, particularly when the infection spreads from nearby structures like the middle ear or sinuses.
Systemic Infections: Sometimes, infections elsewhere in the body can indirectly affect inner ear function through inflammatory or immune-mediated mechanisms.
Autoimmune Reactions: Independent of infections, some people may develop these conditions due to primary autoimmune reactions, where their immune system spontaneously begins attacking inner ear structures.
Recover faster, move better, and feel stronger with expert physiotherapy. Our team is here to guide you every step of the way.

Understanding the typical symptoms of these conditions can help you recognize what's happening and communicate effectively with your healthcare provider. While the experience can be frightening, knowing what to expect often provides some reassurance during a very disorienting time.
The Spinning SensationThe most dramatic and defining symptom is sudden, intense vertigo—but this isn't just feeling "dizzy." True vertigo creates a powerful illusion that either you or your surroundings are spinning or whirling around you. Patients often describe it as feeling like they're on a merry-go-round that won't stop, or as if the entire room is rotating around them.
The Timeline of TerrorThis isn't a brief episode of dizziness that passes in a few minutes. The vertigo typically builds gradually over several hours, reaching its peak intensity during the first day. Once it reaches full force, it can persist continuously for more than 24 hours, often lasting several days without significant relief. This prolonged, unrelenting nature distinguishes these conditions from other types of dizziness.
Movement Makes It WorseAny head movement dramatically worsens the spinning sensation. This is why patients instinctively seek out a dark, quiet room where they can lie perfectly still. Most people find their preferred position: lying on their side with their healthy ear facing down and their eyes closed. Even the slightest head turn can trigger a wave of intense spinning that may persist for minutes.
Severe UnsteadinessThe inflammation disrupts your inner ear's ability to tell your brain which way is up, creating profound balance difficulties. You may experience severe unsteadiness that makes walking feel like trying to navigate during an earthquake. There's often a tendency to fall or lean toward the affected side, as your brain receives conflicting balance information.
The Walking ChallengeDuring the acute phase, many patients find walking alone nearly impossible without support. However, your brain is remarkably adaptable—you can usually maintain sitting balance or stand with your feet spread apart because your brain compensates by relying more heavily on visual cues and sensory information from your feet and joints.
Intense Nausea and VomitingThe constant spinning sensation triggers your body's motion sickness response, often resulting in severe nausea and vomiting, particularly during the first few days. This occurs because your brain interprets the conflicting balance signals as motion, triggering the same response you might experience during severe seasickness. Fortunately, these symptoms typically improve significantly within 1 to 3 days as your brain begins to adapt.
Early Warning SignsInterestingly, about 25% of patients experience brief episodes of dizziness or unsteadiness in the hours or days before the full-blown condition develops. These "prodromal" symptoms might last just a few minutes but can serve as an early warning that something more significant is developing.
Labyrinthitis: The Double ImpactWhen you have labyrinthitis, both your balance and hearing systems are affected because the inflammation involves your entire inner ear. You'll typically experience both the spinning sensation and hearing difficulties simultaneously. This might include hearing loss, ear fullness, or ringing in the ears (tinnitus).
Vestibular Neuritis: Balance OnlyThis is the key differentiating factor: vestibular neuritis characteristically causes severe vertigo without any hearing loss. Your hearing remains perfectly normal because the inflammation affects only the balance nerve, leaving the hearing portions of your inner ear untouched. You won't experience tinnitus, ear fullness, or hearing difficulties.
Rare ExceptionsMedical literature does document uncommon subtypes, such as "inferior vestibular neuritis," where patients might experience some tinnitus and hearing changes. However, these represent unusual variations rather than the typical presentation.
Understanding these differences helps both patients and healthcare providers distinguish between conditions that can initially seem similar.
Duration: Continuous vs. Brief Episodes
Triggers: Constant vs. Position-Dependent
Recovery Pattern: Gradual vs. Immediate
The Practical ImpactThese differences have important practical implications. If your vertigo comes in brief bursts triggered by specific movements, you might have BPPV, which often responds quickly to treatment. If you're experiencing continuous, prolonged spinning that isn't specifically triggered by movement changes, you're more likely dealing with labyrinthitis or vestibular neuritis, which typically require a different treatment approach and have a longer recovery timeline.
If you're reading this while struggling with balance problems, here's what you need to know first: the vast majority of people with vestibular conditions do return to their normal, active lives. While your current symptoms may feel overwhelming, understanding your specific condition and recovery timeline can provide both hope and practical guidance for your healing journey.
Your recovery story will likely unfold in stages, and understanding these phases can help you set realistic expectations:
The Early Recovery Phase (First 3 Months):Most people see their balance issues—particularly the constant feeling of being "off" even when sitting still—resolve during this period with consistent vestibular rehabilitation therapy. This initial phase focuses on helping your brain adapt to the changes in your inner ear.
The Longer Recovery Phase (3-12+ Months):While your day-to-day balance typically improves dramatically, you might notice ongoing challenges with more demanding activities—things like walking in the dark, navigating crowded spaces, or quick head movements during sports. Research shows that a significant portion of patients continue working on these dynamic balance skills well beyond the first year, but this doesn't mean you won't be living normally.
The Long-Term Outlook:Here's the truly encouraging news: 50% to 70% of patients report complete relief from all symptoms when followed up years later. Additionally, recurrence is remarkably uncommon, affecting only a small percentage of patients, and when it does occur, it typically affects the opposite ear rather than the same side.
Your recovery involves two distinct aspects that progress differently:
Your Balance Recovery:Like vestibular neuritis, your balance will improve significantly with proper rehabilitation, following a similar timeline and success rate.
Your Hearing Considerations:The more complex aspect of labyrinthitis involves potential hearing changes. While your vertigo will resolve, some people do experience permanent hearing loss. If this happens to you, it's important to know that modern audiological evaluation and hearing aid technology can provide excellent support, allowing you to maintain your quality of life and communication abilities.
Your return to normal life isn't left to chance—it's supported by a proven, multi-faceted approach:
While the onset of vestibular neuritis or labyrinthitis can feel frightening and disorienting, the combination of accurate diagnosis, targeted medical care, and dedicated vestibular rehabilitation offers a strong, evidence-based pathway back to your normal daily activities. Most people not only recover but regain confidence in their balance and return to all the activities they enjoyed before their illness.
Remember: your current symptoms, however severe, are temporary for the vast majority of people. With proper treatment and time, you can expect to reclaim your normal, active life.
If you're looking for expert guidance through your vestibular recovery, professional vestibular rehabilitation can significantly accelerate your healing process and provide you with the confidence and skills needed for a complete return to your activities.
What Makes Specialized Vestibular Care Different:
While many people do recover naturally, vestibular rehabilitation can be particularly beneficial if you're experiencing:
Look for healthcare providers who offer:
Getting Started:Many insurance plans cover vestibular rehabilitation, and evening or weekend appointments can often accommodate your schedule while you're recovering. The investment in specialized care can dramatically improve both the speed and completeness of your recovery.
Your path to recovery is unique, and having the right professional support can make all the difference in returning to the active, confident life you deserve.
Serving Vaughan, Thornhill, and Toronto. Direct billing available to most insurance providers.
✅ Specialized Vestibular Rehabilitation – Tailored exercises to restore balance and reduce dizziness
✅ 1-on-1 Physiotherapy with Vestibular Specialists – Personalized care from experienced practitioners
✅ Evidence-Based Recovery Plans – Support for both acute and lingering symptoms of labyrinthitis / vestibular neuritis
📞 Call Now: 905-669-1221
📍 Clinic Address: 398 Steeles Ave W #201, Thornhill, ON L4J 6X3
🌐 Online Booking: www.vaughanphysiotherapy.com
Evening and weekend appointments available. Proudly serving Thornhill, Richmond Hill, Markham, Vaughan, and North York communities.
Written by Sophie Lee
Explore the latest articles written by our clinicians