
This comprehensive rehab guide explores conservative management for meniscus tears, including causes, symptoms, tear types, and a detailed 12-week physiotherapy program. Learn how non-surgical treatment can restore knee function, reduce pain, and help avoid surgery for both traumatic and degenerative meniscal injuries.
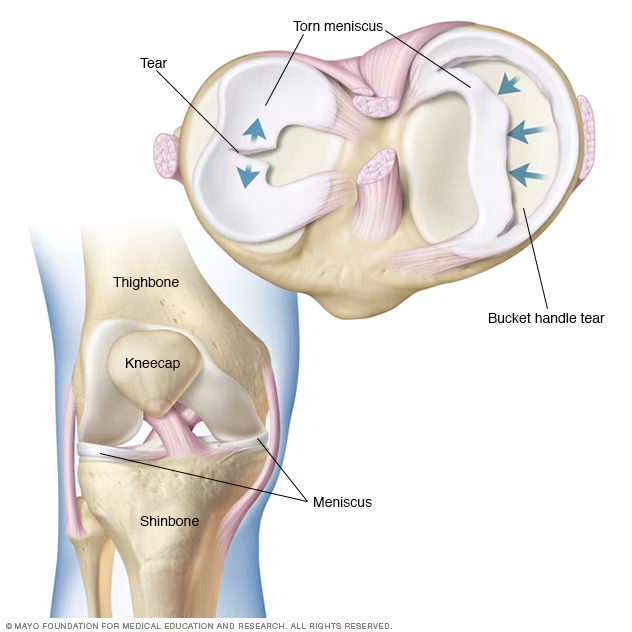
The meniscus is a crucial fibrocartilaginous structure within the knee joint. It is composed primarily of water (72-75%) and collagen (20-28%), predominantly type I collagen, along with smaller amounts of other collagen types, proteoglycans, glycosaminoglycans, DNA, and glycoproteins. The menisci are crescent-shaped wedges situated between the femoral condyles and the tibial plateaus. The medial meniscus is C-shaped and covers about 60% of the medial compartment, while the lateral meniscus is more circular and can cover up to 80% of the lateral compartment surface.
Function of the Meniscus:The menisci perform several vital functions for normal knee operation:
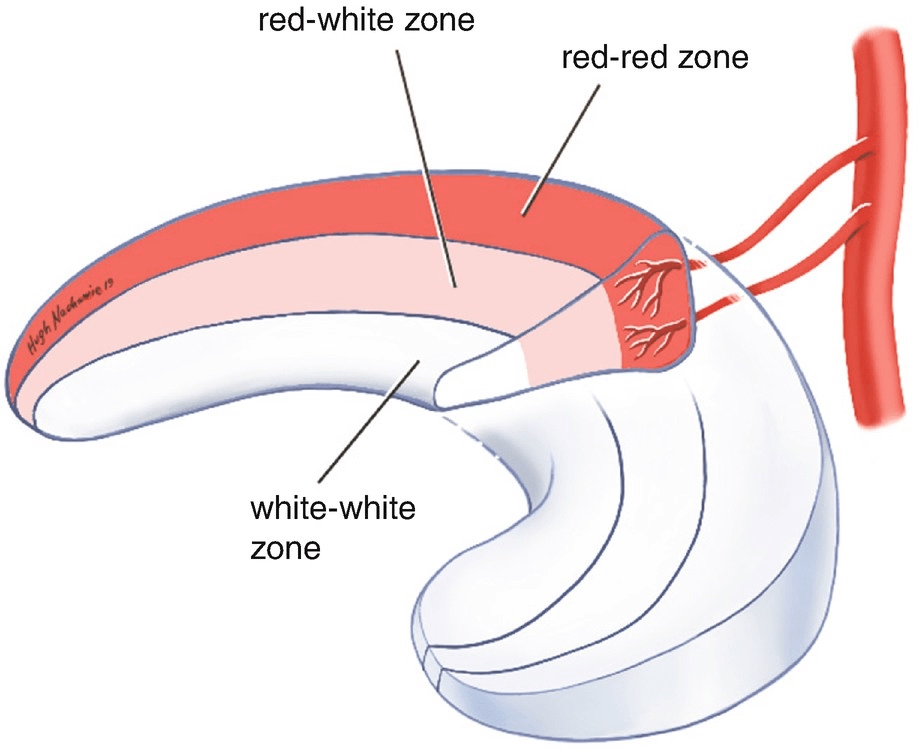
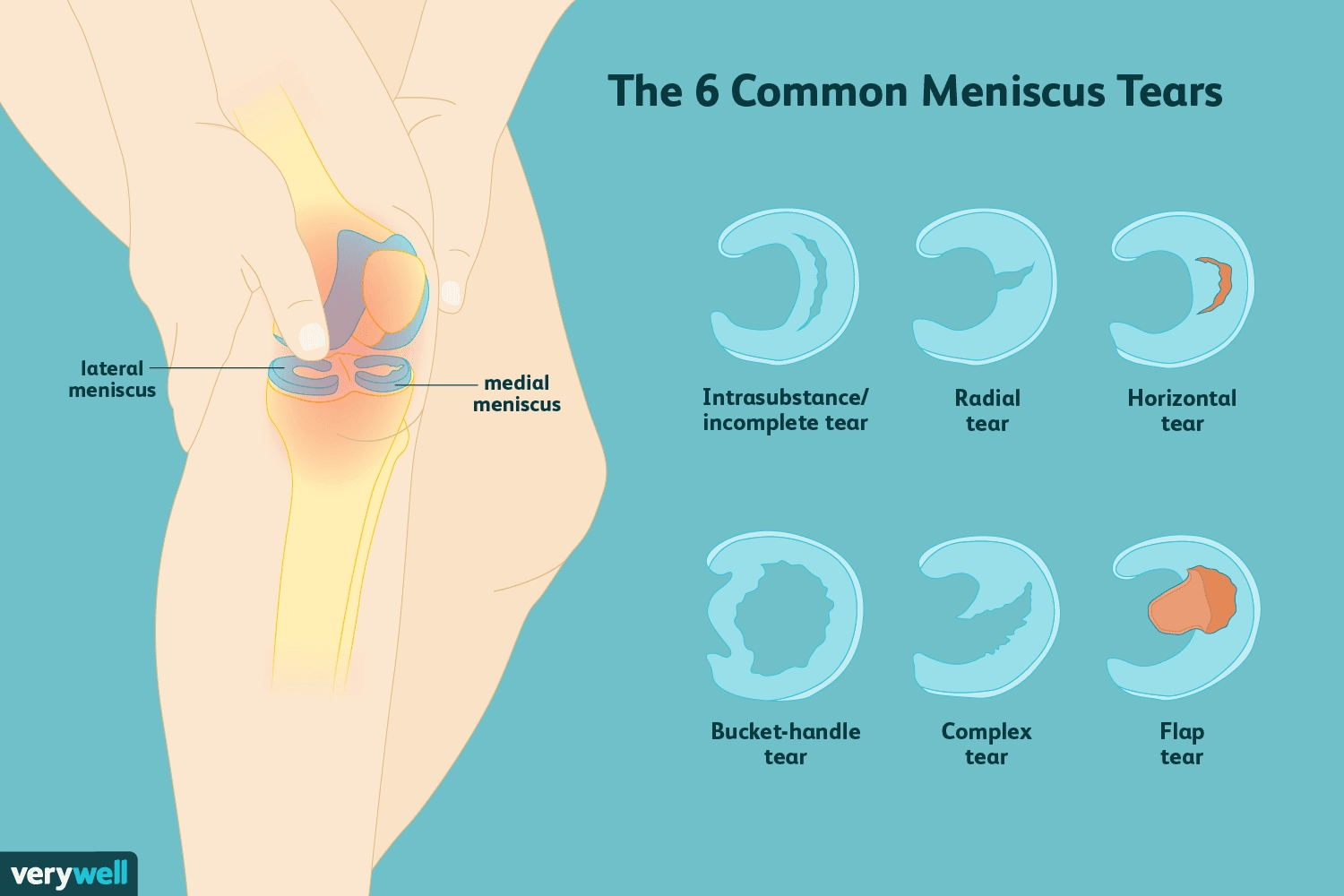
Types of Tears:Meniscal tears are generally classified by pattern (vertical, horizontal, complex), location (radial direction as red-red, red-white, white-white zones), and thickness, as determined by MRI or arthroscopy. The success of meniscal healing is influenced by patient age, time since injury, and tear type.
Common Symptoms:Patients with meniscal tears often report specific symptoms:
A traumatic meniscus tear can cause pain by directly affecting the nociceptors of the meniscus and synovial membrane, and through elevated concentrations of intra-articular cytokines. The presence of inflammatory mediators like IL-6, IL-8, and tumor necrosis factor-α can persist after a tear and suppress meniscal repair.
Yes, a meniscus tear can potentially heal without surgery, especially certain types of tears and in specific patient circumstances. Conservative management, often involving physical therapy, is a primary approach for many patients. Our 12-week rehab program shows 68% success rate avoiding surgery.
Conservative Rehabilitation Effectiveness:
Recovery Timeline:
It's important to note that the presence of inflammatory mediators can suppress meniscal repair even after a tear. While conservative management is a strong first-line approach for many, the optimal treatment strategy depends on multiple factors, including patient demographics and the specific characteristics of the tear.
Conservative management, which often includes physical therapy, is a recognized first-line treatment for knee pain stemming from meniscus tears, both acute and chronic. For degenerative tears, especially those without mechanical symptoms like locking or catching, and for simple traumatic tears, physical therapy is a reasonable and effective initial approach.
While the sources emphasize categories of exercises and therapeutic goals, detailed, specific regimens for nonoperative management of meniscus tears are noted as not being extensively studied in the literature with randomized controlled trials comparing physical therapy with time and rest. However, there is abundant literature supporting the general use of conditioning programs for knee pain and function in knee osteoarthritis, which are extrapolated for meniscus tears.
A typical physiotherapy treatment plan, drawing on the principles and types of exercises mentioned in the sources, can be structured into phases:
Goals: The primary goals during this initial phase are to control and manage swelling and pain, and to restore gentle knee range of motion.
Goals: This phase aims to progress strengthening and improve stability.
Goals: The final phase focuses on restoring full functional capacity, including sport and work-specific movements.
Overall Recovery Timeline and Considerations:Physical therapy can lead to a gradual resolution of symptoms, with clinically meaningful improvements in quality-of-life and pain subscales observed within 12 weeks, and these results often sustained or improved at 1 year. Some studies indicate significant improvement in both surgical and exercise therapy groups after eight weeks, with no significant difference in outcomes between them. The duration of exercise therapy in studies has ranged from 3 to 12 weeks, with most trials adopting the longer 12-week regimen.
If mechanical symptoms persist, are disabling, and significantly affect the quality of life after conservative management (typically after 3 months), surgical intervention may be considered. However, exercise therapy has been shown to provide stable and lasting results over time, with a low rate of conversion to surgery. It is also emphasized that physical therapy is the only approach that can target the joint in its entirety, including extra-articular structures like ligaments, muscles, and tendons. Regular and gradual muscular strengthening, posterior kinetic chain stretching, and proprioceptive exercises are fundamental strategies to prevent strength loss and the onset of flexion contracture, which can worsen knee function and increase pain in a degenerated joint.
Recover faster, move better, and feel stronger with expert physiotherapy. Our team is here to guide you every step of the way.

Q: Is walking good for a meniscus tear?A: Walking can be a part of the rehabilitation process for a meniscus tear, but it should be introduced progressively and cautiously. Initial nonoperative management for an acutely painful and swollen knee with a suspected meniscus tear typically begins with the R.I.C.E. (rest, ice, compression, elevation) principle, and offloading the injured knee might be necessary for comfort. Patients can then progress to full weight-bearing as tolerated. Physical therapy programs often encourage endurance activities like walking and cycling to maintain conditioning, eventually progressing to running and other sport-specific exercises. The goal is to progress to weight-bearing exercises as tolerated. This suggests that while walking is good for rehabilitation, initial limitations, such as avoiding long distances or uneven terrain, would be prudent during the early phases of recovery, aligning with the idea of gradual progression.
Q: Can a torn meniscus heal itself?A: The ability of a torn meniscus to heal itself depends significantly on the location of the tear due to varying blood supply within the meniscus.
Q: Should I wear a knee brace?A: Temporary use of a knee brace may be part of conservative management for meniscus tears. In cases where a nonreducible bucket-handle meniscus tear is repaired, and there's a delay in ACL reconstruction due to an inflamed knee, patients "may wear a brace between the surgeries to potentially protect the menisci". However, the provided sources do not discuss whether long-term reliance on a knee brace can weaken muscles. That specific detail is outside the scope of the given sources.
Choosing a clinic for meniscus rehabilitation involves considering approaches that are supported by current evidence and comprehensive in their offerings. Here's why you might consider "Our Clinic" for meniscus rehab, drawing on the principles discussed in the provided sources:
Evidence-Based Protocols Tailored to Tear Type and Location:The clinic's focus on evidence-based protocols tailored to tear type and location aligns directly with established practices in meniscus tear management.
Advanced Techniques:
Prevention Focus with Neuromuscular Training:A focus on prevention through neuromuscular training is well-supported by the sources.
Serving Thornhill, Vaughan, Markham & GTA:"Our Clinic" serves the Thornhill, Vaughan, Markham, and Greater Toronto Area.
Overall, conservative management including physical therapy is often the initial approach for meniscus tears, especially for those without severe mechanical symptoms or in the more vascularized regions. This approach emphasizes restoring strength, motion, and neuromuscular control to improve function and potentially avoid surgery. If symptoms persist after a proper regimen of conservative treatment, typically after 3 months, surgical intervention might be considered.
Book Your Specialized Assessment Today:
Whether you’re an athlete or active adult, our phased rehab approach helps you recover stronger. Contact us today to begin your personalized recovery plan.
Explore the latest articles written by our clinicians